Respiratory Ward - Swyer-James Syndrome
Cases from the Respiratory ward
Miss NM
17 year old female from Soweto. She presented with a non productive cough of 4 weeks duration. There was no history of chest pain, hemoptysis, shortness of breath or night sweats. She had no previous history of chest problems and she had never smoked. She was otherwise well.
On Examination:
Her vital signs were normal. She was not wasted. There was no evidence of clubbing, cyanosis, or lymphadenopathy. She was apyrexial. On examination of her chest, there was a scoliosis, decreased chest expansion on the left side with accompanying decreased breath sounds and crepitations. The rest of her examination was normal.
Investigations:
Her blood tests including an arterial blood gas were normal. Bronchoscopy revealed inflammation of the left main bronchus with evidence of distal airway dilatation and bronchiectasis and pus in the lumen of the basal segments. Bronchial washings were normal.
Chest X-Ray:

Chest Xray shows evidence of marked scoliosis. There are changes consistent with old fibrocavitatory tuberculosis in the right upper lobe. On the left the lung markings are absent and there is a small cystic lesion in the lower lobe on the left
CT Chest:
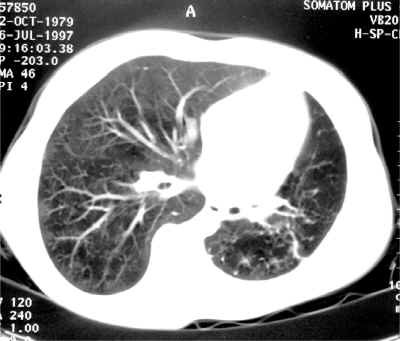
High resolution CT scan of the chest showing a small L hemithorax with small L lung and secondary infection in the LLL with large cavity formation and hyperinflation of LUL. There is also mild bronchiectasis in the left lower lobe and decreased vasculature marking on the left.
SWYER-JAMES SYNDROME (SYS)
Also known as the unilateral hyperlucent lung or Macleod s syndrome. It is an uncommon disease that is considered to be an acquired lesion that follows a number of lung insults, usually in infancy or childhood.
AETIOLOGY
The condition typically follows a lower respiratory tract infection in infancy or childhood. Thus it is a post infectious form of bronchiolitis obliterans following a number of lung insults;
- Infections
- Viral
- Measles
- Pertussis
- Adenovirus
- Bacterial
- Tuberculosis
- Mycoplasma
- Others
- Foreign body aspiration
- Hydrocarbon pneumonia s
- Radiation therapy
- Toxic fumes
- Organ transplantation
- Viral
CLINICAL FEATURES
These tend to be variable and it is often an incidental finding on chest xray. Most patients are asymptomatic in adulthood. Others may complain of a cough, recurrent chest infections, shortness of breath, or hemoptysis.
PATHOGENESIS
This is not clear. Current theory favors a post infectious bronchiolitis obliterans. This follows on repeated infections in early childhood. The consequent bronchiolitis obliterans results in;
- Distal airways trapping, airway distension and eventually changes characteristic of emphysema
- Fibrosis of the lung with reduction in lung capacity and a compensatory reduction in pulmonary blood flow. Because the condition is usually acquired in childhood before the lungs have reached full development, the affected lung or lobe is usually small and hypo plastic
- Bronchiectasis may or may not be present
FUNCTIONAL ABNORMALITY
Evidence of airway obstruction and increase in residual volume is present. There is diminished oxygen uptake in the affected lung. There is also decreased ventilation or blood flow in the affected lung.
DIAGNOSIS
The diagnosis is essentially a radiological one. The syndrome is primarily recognized by it s characteristic radiographic appearance of;
- Lobar or unilateral hyperlucent lung
- Small or normal lung volume on the affected side
- Small hilar shadows
- Sparse intrapulmonary vascular markings
- Air trapping on expiration
Other diagnostic modalities such as bronchoscopy, bronchography, angiography and scintigraphy are also used to rule out other differentials such as;
- unilateral agenesis or hypoplasia of a pulmonary artery
- Massive pulmonary thromboembolism
- Endobronchial tumor
More recently CT scans especially high resolution scans and spiral CT angiography have shown to be valuable modalities in confirming the diagnosis of SJS. It also allows for precise evaluation of vascular, bronchial and parenchymal structures.
CT scan also shows that although classically considered to affect one lung or lobe, the disease may be more heterogeneous in distribution and that contra lateral parenchymal lesions can be present.
TREATMENT AND PROGNOSIS
The prognosis is generally good. Most patients have an asymptotic course unless the opposite lung becomes diseased. The treatment is generally symptomatic. However, surgery should be considered if secondary infection or bronchiectasis become severe.
CONDITIONS THAT MAY PRESENT AS A UNILATERAL HYPERLUCENT LUNG
- Technical difficulties
- Pt rotation
- uneven film development
- Conditions that simulate a unilateral hyperlucent lung
- pectoral muscle absence or wasting
- absence of breast or soft tissue surgery
- scoliosis
- hypolucency of the contra lateral lung
- Parenchymal Aetiologies
- compensatory over inflation
- emphysema
- central obstruction of a bronchus
- Vascular Aetiologies
- pulmonary embolism
- pulmonary artery stenosis or agenesis

