World’s first intentional HIV+ liver transplant
- Wits University
Wits doctors transplanted the liver from a mother living with HIV to her critically ill HIV negative child, who had end-stage liver disease.
Would you rather die of liver failure or live with HIV?
This was the ethical dilemma faced by doctors at Wits Donald Gordon Medical Centre to save a child’s life.
In 2017, doctors from the Transplant Unit at the Wits Donald Gordon Medical Centre performed what is believed to be the world’s first intentional liver transplant from a mother living with HIV to her critically ill HIV negative child, who had end-stage liver disease.
Now, more than a year later, the mother and child have fully recovered, however, doctors are unsure the HIV-status of the child.
 In South Africa, a country with the largest anti-retroviral therapy (ART) programme in the world, people with HIV live long and healthy lives.
In South Africa, a country with the largest anti-retroviral therapy (ART) programme in the world, people with HIV live long and healthy lives.
The success of this world-first operation thus presents a potential new pool of living donors that could save additional lives.
Leveraging “living positive” to save more lives
In a paper published in prestigious, peer-reviewed journal AIDS on October 4, 2018, scientists in surgery, ethics, and HIV from the University of Witwatersrand, Johannesburg (Wits) explain how a chronic shortage of organs compromise their efforts to save lives, and how the decision they made to perform a world-first operation could advance transplantation.
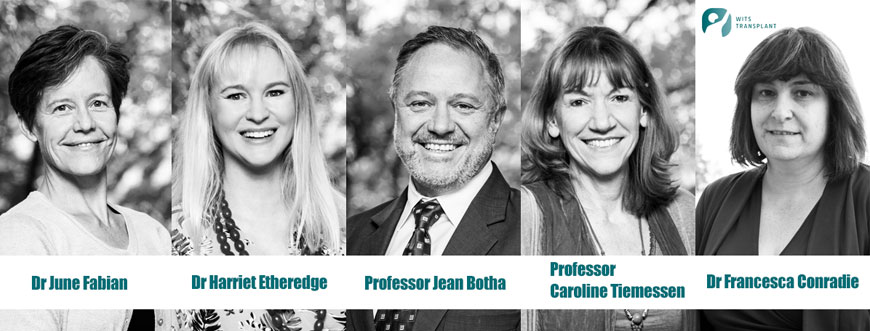
Jean Botha, principal investigator and transplant surgeon is Professor of Surgery in the Department of Surgery in the School of Clinical Medicine, Faculty of Health Sciences at Wits University.
“Two aspects of this case are unique. Firstly, it involved intentional donation of an organ from a living HIV positive individual. Secondly, pre-exposure prophylaxis [medication to protect at-risk individuals from contracting the HI virus] in the child who received the organ may have prevented the transmission of HIV. However, we will only know this conclusively over time,” says Botha, who is also Director of Transplantation at the Transplant Unit at the Wits Donald Gordon Medical Centre.
Currently, the Wits Donald Gordon Medical Centre is the only Transplant Programme doing living donor liver transplantation in southern Africa. It is also the first privately administered teaching hospital in Johannesburg and, as a Wits hospital, advances specialist training and research.
Stringent adherence to ethical guidelines
In this case of transplanting a liver from an HIV positive donor to a non-infected recipient, the transplant team had to unpack the potential risks and benefits to both. The Human Research Ethics Committee (Medical) at Wits University approved the liver transplantation from the mother living with HIV to her HIV negative child. Their personal details remain confidential.
The child – on the waiting list for a deceased donor for 180 days (the average is 45 days) – was frequently admitted for life-threatening complications of end-stage liver disease. Without transplant, the child would certainly have died. However, saving the child’s life needed to be balanced against harm to the donor and the risk of almost certainly transmitting HIV if the mother was the donor.
Dr Harriet Etheredge is a medical bioethicist who holds an honorary position in the Department of Internal Medicine, School of Clinical Medicine at Wits, and oversees Ethics and Regulatory Issues at the Wits Donald Gordon Medical Centre.
“Extensive efforts were made to identify either a deceased liver donor or an HIV negative living donor for the child before considering an HIV positive parent donor. Transplanting HIV positive organs is not illegal in South Africa; however, it is not considered best practice internationally because of the risk of HIV transmission to the recipient. To minimise risk to donors and recipients, this operation is offered only under exceptional circumstances. Full consent is required from the parents who must be able to care for a child infected with HIV,” says Etheredge, whose PhD is in the field of medical ethics and organ transplantation.
In this transplantation case, the mother asked a number of times for the opportunity to save her child’s life by donating a segment of her liver. For this mother, quantifying the risk was simpler for the transplant team. Dr Francesca Conradie, HIV clinician, notes, “When considering an HIV positive parent, it is important that they have an undetectable viral load. This means that they know they are HIV positive and that they have been taking their antiretroviral medication properly for at least six months”.
This made the risk of donation equivalent to that of an HIV negative living donor. However, living liver donation is never a risk-free procedure, and the team took care to ensure that the mother understood the full ambit of the risk she was undertaking.
“Our Independent Donor Advocate helps the parents understand the risks, makes representations to the transplant team on behalf of the donor if necessary, and provides emotional support throughout the process,” says Etheredge.
Intentional transmission of HIV to save a life
The transplant team faced the dilemma of saving the child’s life whilst at the same time knowing that the child might end up HIV positive because of this decision. However, because this intentional HIV positive living donor liver transplant is likely a world first, the actual chance of transmitting HIV was unknown.
The team decided to work on the basis that the child would contract HIV, and provide management accordingly. But in the time since the transplant, there have been some surprises when it comes to the child’s HIV status.
“In the weeks after the transplant, we thought that the child was HIV positive, because we detected HIV antibodies,” says Botha.
The transplant team then accessed specialised testing by HIV experts at the National Institute of Communicable Diseases (NICD) who subsequently could not find any active HIV infection in the blood stream of the child, meaning there is a chance that the child is HIV negative.
Caroline Tiemessen is Research Professor in the School of Pathology at Wits and head of Cell Biology within the Centre for HIV and STIs.
“At the moment, we are developing new methods for testing the child, and we hope to be able to have a definitive answer to the question of seroconversion in future. For now the child will remain on ART until we have a more comprehensive picture,” says Tiemessen who, in 2017, led the laboratory investigations in the case where of a South African child living with HIV had remained in remission without ART since 2008.
Seroconversion is the period of time during which a specific antibody develops and becomes detectable in the blood. After seroconversion has occurred, HIV can be detected in blood tests for the antibody.
Expanded organ donor pool to advance transplantation in Africa
More than a year since the intentional liver transplantation from a mother living with HIV to her HIV negative child, both donor and recipient have recovered and are well.
Dr June Fabian, a nephrologist and Research Director at Wits Donald Gordon Medical Centre says, “We have formalised this procedure as a research programme. As we offer this type of transplantation to more children, we hope to be able to draw more definitive conclusions.”
Organ transplantation at the Wits Donald Gordon Medical Centre is offered to any person irrespective of income or demographic according to “sickest first” criterion. This is possible through an existing partnership between the Wits Donald Gordon Medical Centre and the Gauteng Department of Health.
“We hope that this ground-breaking operation will be the first of many like it and will contribute towards promoting justice and equity in liver transplantation in South Africa,” says Fabian.
ABOUT THE DOCTORS
Professor Jean Botha is Director of Transplantation at Wits Donald Gordon Medical Centre. After completing his general surgical training at the University of the Witwatersrand, Johannesburg, he completed a two-year fellowship in transplantation at the University of Nebraska Medical Center in Omaha, Nebraska where he stayed on as Associate Professor of surgery before returning to South Africa to take up his current position. His main interest is living donor liver transplantation.
Dr Francesca Conradie is a Clinical Research Specialist. She earned her MBBCh in 1989 when the prevalence of HIV infection was around 1%. In addition, HIV infection was a progressive illness that almost invariably resulted in death. In the course of her career, Conradie has seen HIV infection rise to over 30% in Gauteng province where she works and has been part of the research agenda that brought effective antiretroviral therapy to over 3.2 million South Africans. Conradie has participated in drug trials, operational research – including the Comprehensive International Programme of Research on AIDS—South Africa (CIPRA) project 1 – and the pivotal prevention research as part of HPTN 052. This was a randomized trial to evaluate the effectiveness of ART plus HIV primary care versus HIV primary care alone to prevent the sexual transmission of HIV-1 in serodiscordant couples. Her research focus now is on multi-drug-resistant tuberculosis (MDR-TB). She is involved in the registrational clinical trials of the new drug, bedaquiline, and the implementation of its rollout. In 2015, Conradie was appointed Technical Specialist – Clinical Research Advisor at the Union Against TB and Lung Disease, North America.
Dr Harriet Etheredge is a medical bioethicist with a particular interest in ethical challenges across highly specialised medical settings. She joined Wits Donald Gordon Medical Centre in 2015. Etheredge is a Co-Chair of the Wits Human Research Ethics Committee (Medical) and she holds an honorary position in the Department of Internal Medicine, School of Clinical Medicine at Wits University. At a national level, she is a member of the South African Medical Research Council Human Research Ethics Committee (Medical). Etheredge holds a doctorate in the field of medical ethics and organ transplantation and she is a widely published academic author and a public speaker. She was named as one of the Mail & Guardian’s Top 200 Young South Africans in 2016.
Dr June Fabian is a specialist physicianand nephrologist and Director of the Clinical Research Office at the Wits Donald Gordon Medical Centre. She is a joint staff member in the Division of Nephrology, Department of Internal Medicine, University of the Witwatersrand and is actively involved in under- and postgraduate supervision of various research projects. She is passionate about doing research that is relevant and sensitive to the health requirements of South Africans.
Professor Caroline T. Tiemessen heads the Cell Biology Research Laboratory within the Centre for HIV and STIs at the National Institute for Communicable Diseases (NICD), and holds a joint appointment as Research Professor at the University of the Witwatersrand. In 2013, she was awarded the DST/NRF Research Chair of HIV Vaccine Translational Research in the Faculty of Health Sciences at Wits University and was appointed a member of the Academy of Science of South Africa. In 2017, Tiemessen received the prestigious Vice- Chancellor’s Research Award from Wits University. Her research interests include the study of HIV vaccines and HIV cure (paediatric and adult).
FREQUENTLY ASKED QUESTIONS
How long until we know for sure if the child has contracted HIV or not?
Because this has never been done before, we do not have any prior experience. At the moment, the short answer is that we do not know. It is possible that the only way we could find out for sure whether our child has HIV is if antiretroviral therapy (ART) medication was stopped in the child. We are aware that this would be risky, and hope to explore all other avenues of HIV testing first. If we did make such a decision, it would be in full consultation with the parents, HIV experts and the ethics committee. For now, we have agreed to keep the child on ART indefinitely until we have further information. Longer term, to answer these questions, we have obtained approval from Wits Human Research Ethics Committee to conduct a study that will include in depth studies of similar cases that we hope to transplant in the future.
What was done to mitigate risks to the surgeon and theatre staff in terms of transplanting an HIV+ organ?
Conducting surgery on HIV positive people is commonplace, and provided the surgical team wear gloves and masks (which they are required to do for all procedures, regardless of the HIV status of the patient) the risk of transmission is considered very low. We call this adherence to “universal precautions”, which is standard practice. There are no additional precautions required if someone is HIV positive. In the case of this HIV positive mother, risk of transmission was even lower, because the mother had an undetectable HIV viral load. This means that there was very little active virus in the mother’s body and the chance of the surgeons being infected was very small.
HIV is a sexually transmitted infection. Does HIV ‘live’ differently in the liver as opposed to other organs? How?
Not much is known about how HIV ‘lives’ in the liver of humans. The liver itself is an amazing organ; it regenerates, which means that it can grow back. Scientists have looked at the way that HIV ‘lives’ in the liver of monkeys. The scientists found that in 42 monkeys infected with simian immunodeficiency virus (SIV) – the monkey-version of HIV – there was productive SIV infection in the liver of only one animal, whereas in contrast other tissues (jejunum, colon, lymph nodes) of all animals had high numbers of infected cells. Although we cannot always say that things will be the same in humans as they are in animals, this research does suggest that HIV might not ‘live’ in the liver as much as it does in other organs and tissues. We will be investigating this in a much more in-depth way as we continue our research with future cases.
Is HIV+ and liver failure a co-infection in the same way that HIV and TB is? OR Are more people HIV+ than those in need of transplants?
In our liver transplant programme at Wits, HIV itself has not caused more children to develop liver failure. For most children who require a liver transplant, the cause of their liver failure is a condition called biliary atresia, which has nothing to do with HIV. Biliary atresia is a condition that children are born with and many die without it being diagnosed or, if it is diagnosed, the children are not referred for transplantation.
In our adult liver transplant programme, we have performed some transplants due to acute liver failure from efavirenz (an antiretroviral medication), which occurs in a minority of people taking ART.
What is the incidence of HIV+ in those requiring transplants?
In our liver transplant programme, the incidence is very small. HIV status does not exclude one from transplantation, provided the HIV is well controlled, i.e., HIV viral load is suppressed, CD4 count is above 200 and there is no active TB infection.
There is potential of a new living liver donor pool. Is this specifically a pool of HIV positive donors or all donors?
Because the liver has the capacity to regenerate, living donation using a portion of the liver is a well-established procedure worldwide. The inclusion of HIV infected people as living donors created the new living donor pool. This is particularly relevant in South Africa, where we have a high prevalence of HIV infection and a very good ART treatment programme – which means donors living with well-controlled HIV, can potentially be donors.
Before this case, we would not have usually considered HIV positive people as living donors, because there are some risks of the surgery. However, in this single case we have shown that when the donor has well-controlled HIV, is taking their medicine properly, and does not have any other illness, then it is safe for an HIV positive person to be a living donor.
HIV positive persons can often be deceased donors, especially in the donation of kidneys from HIV positive people to other HIV positive people. However, this is not the ‘new’ donor pool that is referred to in our research.
If the recipient remains HIV negative, are you able to say why?
In the long run, we might be able to work out why this could be the case. It will involve further study of the drugs used to prevent HIV, the way HIV ‘lives’ in the liver and the way the HIV is transmitted.
What are the mortality implications of living both with a transplanted liver and with HIV? And of living with a transplant of a HIV negative liver?
Patients with HIV are no longer excluded from getting transplants and research suggests that the outcomes are the same regardless of whether the recipient has HIV or not.
Will a transplanted liver react differently to ARVs than an ‘original’ liver?
No, it works exactly the same.
Intentional transplant of organs from HIV+ living donors is not universally accepted as best clinical practice. Is it more the HIV+ that is the problem or the fact that the donor is living?
The donation of a portion of liver from a living donor to a recipient is well established, with very good results internationally and it is accepted as good clinical practice. It is the HIV+ factor that has made some transplant centres wary of the potential risks involved.
Your transplant programme usually excludes HIV+ donors because it puts the donor at risk. How? Surely the recipient is more vulnerable?
There might be more complications related to the surgery if a donor has uncontrolled HIV. By this, we mean a high viral load, and potentially low CD4 count and this places the donor at risk, for example, of getting wound infections. Research has shown that if HIV is well controlled, i.e., The CD4 count is above 200 and the viral load is undetectable, then the risk for the donor is the same as someone who does not have HIV infection.

FACT SHEET
Paediatric liver transplantation at the Transplant Unit of Wits Donald Gordon Medical Centre:
- In 2017, 14 children who were on the waiting list for a liver transplant in Johannesburg died before they could be transplanted
- The Transplant Unit at the Wits Donald Gordon Medical Centre is the largest volume paediatric liver transplant unit in South Africa and the only unit in sub-Saharan Africa that offers living donor liver transplantation for children
- Most of the children who need a transplant suffer from a condition called Biliary Atresia, which is a condition present from birth. The only cure is through liver transplant
- Eighty percent of all the children who receive a liver transplant are alive one year after the transplant operation took place. This is in line with the survival seen at international transplant centres
- The Wits Transplant Unit offers care to any child in South Africa who is in need of a liver transplant, regardless of whether they are referred from a state or a private facility
- Over the last five years, Wits has performed over 130 liver transplants for children with liver failure

A BRIEF HISTORY OF HIV ORGAN TRANSPLANTATION IN SOUTH AFRICA
Organs for all
Since 2013, the transplant programme at Wits Donald Gordon Medical Centre has seen a dramatic increase in the number of children on the waiting list for organs. This may be due in part to increased awareness and better referral patterns, but also because liver transplantation has been made accessible to all children who need this form of therapy, regardless of payer-status. This is made possible through a partnership developed over many years between the Wits Donald Gordon Medical Centre and the Department of Health.
But not enough organ donors
However, the availability of organ donors has not kept pace with the growing demand for transplants. This means children die while waiting for organs. For children in South Africa with end-stage liver failure, the only treatment option is a liver transplant. For this to happen, a liver can be sourced from deceased donors, but the shortage of deceased donors in this country makes it very difficult to find enough donor livers for the children who need them.
Alternative organ sources
This critical organ shortage necessitates exploration of alternatives for patients. Thus, the Wits Donald Gordon Medical Centre established its living donor liver transplant programme in 2013 with the assistance of colleagues from Omaha, Nebraska. This is the only programme of its kind in sub-Saharan Africa. This programme opens up an additional source of liver donors – living people. Living people can donate a portion of their liver because the liver regenerates. Anyone who is in the position to be a living liver donor needs to meet strict medical criteria, undergo extensive education and consent to the surgical procedure. This means that not all people can be living liver donors, even if they want to.
How to transplant a liver from a living donor to a child recipient
- A portion of the liver is taken from the donor - usually a parent
- This portion is given to the child
- As the child grows, the liver also grows, which ensures that they are healthy
- The donor’s liver regenerates to its normal size within about six weeks, so ultimately the donor is not compromised. However, the surgery to remove the liver segment from the donor does come with some risks, as do all surgical procedures.
Whilst patients undergoing a liver transplant will experience an excellent quality of life, this does not means that they will then be free of health complications. For this reason, people who have had organ transplants are followed-up very carefully by the medical team.
When the living donor liver transplant programme began at Wits Donald Gordon Medical Centre, colleagues at the University of Cape Town – motivated by similar organ shortages and lack of access to dialysis for kidney failure patients – started performing kidney transplants from HIV positive deceased donors into HIV positive recipients, with good results. Based on the success of the Cape Town programme, the HIV Organ Policy Equity (HOPE) Act was signed into law in the USA in 2013. The HOPE Act permits the transplantation of organs from HIV positive individuals.
A plea from parents
Whilst South Africa has the highest global prevalence of HIV, we also have the largest treatment programme in the world, thanks to the efforts and commitment of the SA government. The success of the prevention of mother-to-child transmission of HIV has resulted in a population of healthy young adults living with well-controlled HIV who have HIV negative children. It is these parents, presenting at the transplant unit of the Wits Donald Gordon Medical Centre with children in liver failure, who have challenged why their HIV positive status excludes them from being living donors and saving the lives of their children.
For this reason, and subject to rigorous ethical regulations, this operation was performed in 2017, making the transplantation of a liver from an HIV positive mother to her HIV negative child a life-saving world first.
The need for organs for transplantation is high and presently unmatched by the availability of donor organs. People die waiting. This growing demand, coupled with the knowledge that people with HIV can live long and normal lives on antiretroviral therapy ART, and the lessons learnt from the transplant may open up another potential therapeutic option for those in need of life-saving organ transplants.

About Wits Donald Gordon Medical Centre
Wits Donald Gordon Medical Centre is a privately administered teaching hospital in Johannesburg. The primary function of Wits Donald Gordon Medical Centre is to provide specialist and sub-specialist training to doctors, hence supplementing the training available in the state health sector. The type of training provided includes super-specialised surgery, pediatrics, hepatology, oncology and a number of other fields. The financial model of Wits Donald Gordon Medical Centre is structured such that all profits made through the daily running of the hospital are channeled back into training, teaching and supporting programmes like transplantation. This allows Wits Donald Gordon Medical Centre to subsidise the provision of specalised health services, like transplantation, to state sector patients. This goes some way towards promoting the principles of equal access in within the South African health system.

